Background: Primary cerebral lymphoma (PCNSL) is a rare subtype of diffuse large B-cell lymphoma (DLBCL) with a particularly poor outcome compared to systemic DLBCL. Several prognostic scores have been developed for PCNSL. These include the International Extranodal Lymphoma Study Group (IELSG) score with five prognostic factors (patient age, serum lactate dehydrogenase [LDH] level, Eastern Cooperative Oncology Group performance status [PS], deep brain involvement and cerebrospinal fluid [CSF] protein level), and the Memorial Sloan-Kettering Cancer Center (MSKCC) score, which is based on age and the Karnofsky Performance Score (KPS). However, the reproducibility of these two scoring systems is low, and the IESLG score requires CSF protein and LDH levels evaluation, which are not often available. None of these scores incorporate data on nutritional status, in particular albumin, which has been shown to be an important prognostic factor in systemic DLBCL. In addition, a recent study demonstrated that the muscle density and mass determined by imaging segmentation, were strong prognostic factors for newly diagnosed systemic DLBCL patients (Jullien et al. Cancers 2021). Our aim was to determine whether these imaging data were also predictive factors for outcome in newly diagnosed diffuse large B-cell PCNSL patients.
Methods: For each patient included in the study, muscle mass and density were estimated using skeletal muscle index (SMI) and mean skeletal muscle radiation attenuation (SMRA), respectively. SMI and SMRA were computed at L3 level using the whole-body scan (WBS) performed at the diagnosis of PCNSL, by the mean of an automated segmenting algorithm. Muscle characteristics were then classified as normal or low using already validated cut-off according to patients' age and body mass index (Westenberg et al. Sci Rep 2023). Patients' outcomes were then compared based on their muscle quality, albumin level at diagnosis and other clinical variables commonly included in PCNSL prognostic scores.
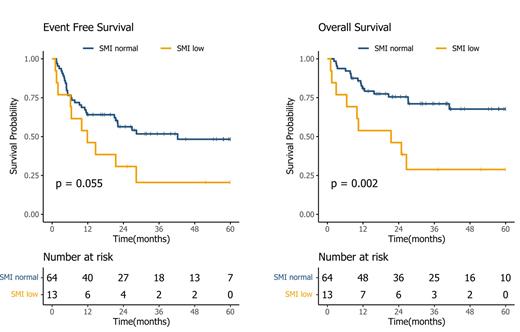
Results: Between 2015 and 2022, 98 consecutive diffuse large B-cell PCNSL patients were newly diagnosed at Hematology Department of Hospital Lyon Sud, France. Among them, 77 had WBS at diagnosis with available data for this study. The median age was 69 years (range 24-87) and 22 patients (29%) presented an altered ECOG PS (PS 3-4 score). All patients were treated with first-line high-dose methotrexate-based chemotherapy in combination with rituximab. SMI was normal in 64 patients (83%) and 17 patients (17%) had low SMI. Patients with low SMI had more frequently an altered PS (p=0.07) and had lower albumin level (mean 36.7 g/L vs 32.0 g/L, p=0.007). SMRA was normal in 30 patients (39%) and 47 patients (61%) had low SMRA. Patients with low SMRA were older (60 vs 70 years old, p=0.001). In univariate analysis, patients with low SMI had worse outcome with significantly shorter overall survival (p=0.002, median OS, 21.4 months vs not reached) and a trend towards shorter event-free survival (p=0.055, median EFS, 11.9 months vs 42.3 months, Figure 1). No significant prognostic difference was seen for SMRA for EFS or OS. The multivariate analysis showed that SMI (Hazard ratio [HR]=3.33, 95% confidence interval [95%CI]= 1.21-9.20, p=0.02) and age (HR =1.86, 95%CI =1.15-3.0, p=0.012) were strongly associated with OS but not tumor localization (HR =1.46, 95%CI =0.60-3.55, p=0.4), PS (HR = 1.54, 95%CI =0.65-3.65, p=0.32) and albumin level (HR =1.05, 95%CI =0.47-2.32, p=0.91). Age was significantly associated with EFS (HR=1.4, p = 0.04) with a more limited association of SMI with EFS (HR=2.03, p=0.095). In exploratory subgroup analyses, we showed that SMI still influenced OS in patients with PS 4 (10 months vs not reached, p= 0.002), suggesting that SMI may be a more appropriate prognostic factor than PS, especially for patients with motor deficit for whom PS is difficult to estimate.
Conclusions: This retrospective analysis of newly diagnosed PCNSL patients showed a significant association between decreased muscle mass, measured by SMI and overall survival, after controlling for other prognostic variables. These findings warrant confirmative analyses to explore the relationship between muscle mass/density and diffuse large B-cell PCNSL patient's outcome and integrate SMI in PCNSL prognostic scores.
Disclosures
Safar:janssen: Honoraria. Sesques:KITE/GILEAD , BMS, JANSSEN, NOVARTIS, CHUGAI: Consultancy. Karlin:Amgen, Celgene, GSK, Janssen, Takeda: Consultancy; AbbVie, Amgen, Celgene, Janssen, Sanofi, Takeda: Honoraria. Salles:Debiopharm: Consultancy; BeiGene: Consultancy; Kite/Gilead: Consultancy; Orna: Consultancy; Nurix: Consultancy; BMS/Celgene: Consultancy; AbbVie: Consultancy, Honoraria; ATB Therapeutics: Consultancy; Janssen: Consultancy, Research Funding; Incyte: Consultancy; Genmab: Consultancy; Genentech, Inc./F. Hoffmann-La Roche Ltd: Consultancy, Research Funding; Ipsen: Consultancy, Research Funding; Nordic Nanovector: Consultancy; Owkin: Current holder of stock options in a privately-held company; EPIZYME: Consultancy; Loxo/Lilly: Consultancy; Merck: Consultancy, Honoraria; Novartis: Consultancy; Molecular Partners: Consultancy. Bachy:Hospices Civils de Lyon Claude Bernard Lyon 1 University: Current Employment; Pfizer: Honoraria, Other: Personal Fees; Takeda: Honoraria; Incyte: Honoraria; Novartis: Honoraria, Other: Personal Fees; Bristol Myers Squibb: Honoraria, Other: Personal Fees, Research Funding; Amgen: Research Funding; Roche: Consultancy, Honoraria; Kite, a Gilead Company: Honoraria, Other: Personal Fees. Ghesquieres:Gilead, Roche: Consultancy; Gilead, Roche, BMS, Abbvie: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal